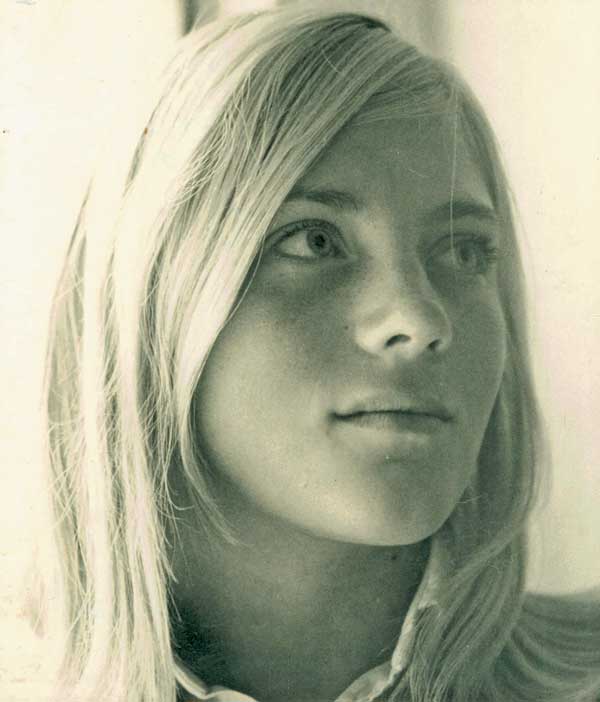
Susanne Long was my sister, three years younger. She was funny and savvy. She was creative and kind and curious. She had a master’s degree, and she taught English as a second language in Washington, D.C., and later in Seattle. She spent two tours of duty in the Peace Corps, one in Liberia, the other in Morocco. She baked, cooked, knitted, quilted, played recorder. She took photographs. She loved to learn languages, and she loved to garden. She trained as a marathon runner. She was happily married, then unhappily married, then divorced. She was a great beauty, with high cheekbones and a Queen Nefertiti nose. She loved to hang out with her friends.
At the age of 32, never before, schizophrenia came to call. She began to hear nasty phrases hissed at her: We’re going to get you, etc. We may call them voices, but to her they were sentences spoken from the mouths of colleagues and passersby.
Over the next near-decade her delusional states increased from sporadic to chronic. On July 21, 1986, at the age of 40, she vanished.
She’d been a voluntary resident at a mental health clinic not far from our parents’ home on the Eastern Shore of Maryland. Our father had taken her out to lunch. She had signed back in. Our mother arrived to take her out to dinner. She was not there. The staff had decided, sign-in notwithstanding, that she was still out with our father. System breakdown. Hours had passed.
Later, one of the other residents recalled how she’d said goodbye to my father. She had flashed him a smile—a beautiful, almost angelic smile.
We and the sheriff’s office conducted a nationwide search, plastering telephone poles and homeless shelters with missing-person posters. My father, with his dogs, searched the deep, tangled, marshy woods near the clinic. The weeks went by, and we could not find Susanne. I was in Boston for the summer, and I organized my friends to plaster the city with posters. Have you seen Susanne? No one had seen Susanne.
That fall, in those woods, on November 7, 1986, two hunters, believing they had downed a white-bellied doe, came across my sister’s white bones. No one knows exactly what happened, but there was no suggestion of foul play. It was a probable suicide.
As the years and decades go by, grief devolves from acute to customary. It does not end. And neither do my questions about schizophrenia. What causes this devastating mental illness?
It’s related to genetics, we know that. If you have an identical twin with schizophrenia, your chances of getting it are 40 to 65 percent. If you have a parent, brother, or sister with it, your chances are 10 percent. This compares with about one percent of the world population that suffers from the illness. One percent, though, is not a small number; in the United States it amounts to about three million people. The most severely afflicted find it difficult to get up, get dressed, eat, go to work, come home. They barely function. Susanne, once intelligent and competent, graceful and well appointed, could no longer keep a job or even take a bath. So why didn’t natural selection, over thousands of years, cause the genetic propensity for this extreme disability to die out?
The genetically inherited disease sickle cell anemia persists because it provides protection against malaria. Could there be an analogous relationship between schizophrenia and imagination?
If imagination is put on a continuum from high to low, people afflicted with schizophrenia are on the high end. Their imaginations fire up to the point of hallucination. Creative persons who are less crazy also imagine what is not there, but they create art or social revolution or a dinner party. (People with schizophrenia can also be quite creative before the disease takes its toll. Susanne loved to draw, paint, and make batiks.)
Imagination, suggests Princeton molecular biologist Lee M. Silver, is related to the brain’s “noise” (random firings of neurons, or nerve cells), thus generating more associations. Brain scans of people with schizophrenia and their unafflicted family members show mega-amounts of random noise. Brain scans of control subjects (no schizophrenia in the family) do not.
A recent major study confirmed a high association between people in creative professions and their first-degree relatives (parents, offspring, and siblings) who have psychopathologies such as schizophrenia. Could there be inherited brain structures that produce thought patterns such as “broad associative thinking” in which contradictory images and ideas knock about together, structures that serve an artist’s work but that in some brains go too far and become the twisted thoughts of mental illness? Does selection for a more robust imagination—so very useful to us humans—keep imagination’s more dysfunctional forms from dying out?
Inflammation—the body’s immune response to injury or infection—is strongly associated with schizophrenia. People with schizophrenia have, it seems, an oversupply of the neurotransmitter dopamine in their brains. In response to inflammation, the immune system produces the protein interleukin-1 beta, which has been shown to upset the dopamine system of rats. Scientists have found raised levels of interleukin-1 beta in the spinal fluid of patients recently diagnosed with schizophrenia. What causes the inflammation that revs up interleukin-1 beta? What are their immune systems responding to?
People born in winter or early spring (flu season) are likelier to develop the illness. (Susanne was born on March 26.) The deranged state can come and go, rather like a chronic infection. These facts led psychiatrist and longtime schizophrenia researcher E. Fuller Torrey to think virus. Another researcher found a certain retrovirus (called HERV-W) in people with multiple sclerosis. (Retroviruses infect cells but let them live.) HERV-W exists in the DNA of every one of us. Stacks of proteins lock it down, tie it up, but in some people it slips out and acts up. And it turns out that patients with schizophrenia have HERV-W in their blood and brain fluid. In multiple sclerosis, the virus may attack brain cells directly, causing paralysis. In schizophrenia, the inflammation may damage neurons indirectly by overstimulating them. Flu during pregnancy—that was our mother with Susanne—can stir it up.
Or, a cat can stir it up. Not the cat itself, but a parasite that cats carry and excrete in their feces, Toxoplasma gondii (Toxo for short). This parasite messes with the brain, causing rats, for instance, to feel a fierce attraction to its predator, the cat. The cat eats the adoring rat, and the parasite returns to the only place it can reproduce: the gut of the cat. The parasite, which enters our own bodies via contact with cat feces, makes cysts in the brain. It has two genes that enable it to crank up the dopamine in the host’s brain. (However, many people infected with Toxo do not have schizophrenia.)
Torrey favors the cat/Toxo theory. Schizophrenia, he says, began cropping up in the late 1700s when a craze began for keeping cats as pets, particularly among “poets and left-wing avant-garde Greenwich Village types.” (But wait. The ancient Egyptians loved their cats. And what about the so-called witches of the Middle Ages, burned at the stake with their beloved cats?) In any case, since the 1950s, some 70 epidemiology studies have explored a relationship between psychosis and Toxo. Susanne adored her cat. Did the cat have Toxo? Did she?
Possibly the brains of persons suffering from schizophrenia have not an excess of dopamine but a deficit of glutamate, a neurotransmitter crucial for learning and memory development. Dopamine receptors inhibit glutamate release. This may explain why, though antipsychotic drugs shut down dopamine receptors soon after the first dose, the voices and delusions don’t vacate for two or three weeks. It may take that long for the brain to crank up glutamate production.
Susanne detested the antipsychotic drug Haldol (haloperidol) and once told me she’d rather be dead than be on it. The drug deleted her terrors but also every other feeling. On Haldol she felt nothing at all.
There’s no single schizophrenia gene but rather a crowd of suspects, as many as 600 possible crazy-making genes. One of them is named DISC1—Disrupted in Schizophrenia 1—but even disc1 is not disrupted (mutated) in all persons diagnosed with schizophrenia. In addition to suspect genes, there’s another genetic characteristic strongly associated with schizophrenia: copy number variants (CNVs), in which parts of certain genes are deleted (or sometimes duplicated). But nothing genetic found so far is even remotely sufficient to explain the strong inherited propensity to develop schizophrenia.
Particular gene variants are linked to both autism spectrum and schizophrenia spectrum disorders (as well as bipolar disorder), which likely explains why these disorders often occur in the same family. A now-discredited theory held that maternal coldness—a mother’s emotional distance and a lack of empathy—led to schizophrenia in a child. If autism and schizophrenia spectrum disorders run in families, could it be that some of those “cold” mothers were autistic? Our professorial mother was brilliant, but her personality was not the warmest or the most expressive. Some of us think she may have had Asperger syndrome, the high-functioning form of autism. (After we were grown, Mother became a psychologist; she spent the last years of Susanne’s life researching schizophrenia and desperately trying to save her.)
Some researchers point to a flaw in all these gene studies. A diagnosis of schizophrenia is tricky and a bit subjective. When you consider a group of people with “schizophrenia,” do they all have the same thing? And if they don’t, what does it mean to search for what they have in common in their genomes? Wouldn’t it be better to study gene variants in relation to narrower traits and symptoms—say hallucinations, which can visit people with different diagnoses or with no diagnosis?
Epigenetics—the way genes switch on and off—is another area of intense interest for schizophrenia researchers. Every nonreproductive cell in our body contains our entire genome, and in every cell, some genes are properly switched on and others off. We inherit our genes, but environment strongly affects the switching mechanisms. This was dramatically demonstrated in a study of persons born during the “Dutch Hunger Winter” of 1944–1945—a famine the Nazis created in the Netherlands by cutting off food supplies in retaliation for Dutch participation in the resistance. Infants born during the famine to half-starved mothers, a cohort now turning 70, have higher rates of all kinds of pathology, including schizophrenia.
The old debate between nature and nurture has become foggy and confused because now we know how much nurture affects nature. Environmental stress, especially in utero but also after birth, alters not our genes but their expression, the switches that turn them on and off. Environmental stress can come from starvation or from toxins such as insecticides or polluted air or water. It can come from recreational drugs or from the stress of traumatic violence.
A new hypothesis suggests that schizophrenia is a developmental disorder, which involves epigenetics—that switching business. Our brain with its 100 billion neurons begins developing in utero but is not fully formed until age 25 or so. Brain development involves neurons migrating from their place of origin to their destination (neuron pruning is also involved). The trip is set in motion by a gene switching on. If there were a glitch in this switching mechanism, it would not become apparent until adolescence, when brain development goes into high gear, and also when schizophrenia commonly flares up. This new insight is promising, but it doesn’t quite capture Susanne’s case, since she was in her early 30s when the disaster arrived.
Back to dopamine. One hypothesis posits that the brains of people with schizophrenia have lost the ability to suppress excess information. In these hyperstimulated brains, dopamine, the key to encoding what’s important and what’s not, encodes random data as meaningful. Two University of Texas computer scientists programmed a voice-recognizing computer with neural networks and taught this artificial brain simple stories. They then simulated a hyped-up dopaminergic system by reducing its ability to forget or ignore. This unfortunate computer became delusional. It made up wild, disconnected stories, even claiming credit for a terrorist bombing. If computers can go crazy, can they be cured? If computers can be cured, can we be cured?
People with schizophrenia commonly chain smoke. Susanne was rarely without a Winston cigarette in her hand, and I used to enjoy having a smoke with her. According to a 2004 publication from the World Health Organization, dopamine runs amok in parts of the schizophrenic brain, but there’s too little of it in the prefrontal cortex, likely contributing to cognitive deficits. But nicotine, it turns out, stimulates dopamine production in the prefrontal cortex—dopamine that these particular smokers badly need. Should stringent antismoking laws take pity on these ill persons who live in agony? Shouldn’t we let them smoke? (Or, maybe, give them a nicotine patch.)
Once, to escape her whispering persecutors, Susanne surreptitiously packed a small bag, took a taxi to the airport, paid the full same-day price for an airline ticket, and flew to Seattle, to the home of our younger sister, Liz. Susanne thereby abandoned her life in Washington, D.C., her apartment, her excellent job as a language teacher. In Seattle she felt safe—for a short time.
The delusion of the death threat is the common coin of paranoid schizophrenia. (Susanne and I were close, and the first few times she revealed to me the terrible things her colleagues were saying to her, I was shocked. I also believed that her colleagues were actually saying these things to her.) How interesting that many people with schizophrenia, people who have neither met each other nor read the same books nor seen the same movies, have virtually identical “voices,” or thoughts. What is going on in their biological, physical brains that produces such eerily similar thinking?
Terror implicates the amygdala, the walnut-sized structure in the brain that makes us feel fear. The rare person born with damaged or absent amygdalae feels no fear, which routinely puts him or her into grave danger. The amygdala gives us fear itself, not the story explaining the fear. Could it be that fear comes first, and the death-threat story is how the brain explains the fear? Could paranoid schizophrenia be a disorder of the amygdala?
We’ve all felt in desperate jeopardy when in reality we were safe and sound—while sleeping, having a nightmare. Rapid eye movement (REM) sleep, which occurs roughly five times per night, is characterized by vivid dreams or nightmares involving a story. These bizarre dream scenarios are entirely believable to sleeping persons. If REM sleep occurred during our waking hours, we would all be certified lunatics. Well. One sleep researcher has considered the ways in which the brains of persons suffering from schizophrenia and those of persons in REM sleep are remarkably similar. In both, the primary visual cortex, which receives images from the outside world via light waves, is inactive, as are parts of the prefrontal cortex related to logic and decision. In both, visual association areas are aroused (vivid dreams or waking hallucinations). In both, the limbic cortex is aroused (emotion). In both, dopamine (desire) is doing its dance and norepinephrine and serotonin (attention and problem solving) are taking a nap.
One afternoon, visiting Susanne in her Seattle apartment, I was reading a novel on her sofa while she was dealing with the terrifying fact (according to her) that the entire Red Chinese army was attacking the apartment. She became incensed that in such an emergency I was reading a book! In her brain, was the switching mechanism between sleeping and waking broken?
In schizophrenia the negative symptoms, as they are called, are devastating. Dull hours of sitting in silence. The loss of curiosity, energy, happiness, hobbies, projects, anticipations, pleasures, enjoyments. The loss of the old skills. The loss of the old and very funny sense of humor. The loss of interest in hygiene. My beautiful sister, gone from lovely to slovenly, from kind, energetic, sweet, and funny to a thick kind of silence. Doesn’t this sound a bit like clinical depression? Am I surprised that a study reported in a 2013 article in Nature Genetics finds a medium-sized correlation between schizophrenia and major depressive disorder?
Schizophrenia is bad enough without cognitive decline. Upon autopsy, cortical thinning is commonly found in the brains of schizophrenic patients, and cortical thinning correlates with cognitive deficits. But what causes this thinning? An excellent longitudinal study of about 1,000 babies born in one year in one hospital in Dunedin, New Zealand, confirmed that over the next four decades, the three percent of this cohort that developed schizophrenia underwent cognitive decline, particularly in what is known as fluid cognitive abilities—processing speed, learning, and executive function. (“Crystallized” abilities, such as verbal IQ , did not change.) According to another study, of some 100,000 adults in Iceland, certain CNVs (those stretches of DNA either repeated or deleted) strongly associated with schizophrenia but found in people without schizophrenia are associated with similar, if milder, cognitive problems.
But consider. Cognitive activity (learning, socializing) is a known preventive of cognitive decline. Also, stress causes a spike in the stress hormone cortisol, which if chronically churned up is known to contribute to dementia by damaging the hippocampus. Could it be that years spent sitting and staring at the wall—along with the chronic stress created by threatening voices—are plenty enough to cause cortical thinning and cognitive decline, no further explanation required?
Yet another theory has to do with the left and right hemispheres of the brain. Both hemispheres are involved in all mental functions—language and image—but, according to Iain McGilchrist in The Master and His Emissary, differently. Speech and semantic language are lateralized in the left hemisphere in about 89 percent of people “in the West at present” and in about five percent of people this is reversed: it makes no difference. But some people “have a partial inversion of the standard pattern, leading to brain functions being lateralized in unconventional combinations.” This can lead to pathologies such as schizophrenia, bipolar disorder, and autism, but also to unusual talents, which, McGilchrist posits, is why the disorders have not, evolutionarily speaking, died out. Is weird lateralization related to early brain development? Is it genetic? Is it epigenetic?
Susanne was never violent; neither did she ever threaten violence, nor were her actions and attitudes in any way aggressive. Most people with schizophrenia are not violent, stereotype notwithstanding. However, in his 2013 book, American Psychosis, Torrey reports that 10 percent of homicides in the United States are committed by untreated mentally ill people. Keyword untreated. And often untreated and drug addicted. That means that 90 percent of homicides are committed by the allegedly sane. But suicide is different. About one in 10 people suffering from schizophrenia commits suicide, according to the National Institute of Mental Health. This compares with about one in 100,000 in the general population. Do people who commit suicide have any idea how devastated their survivors will be? Did Susanne?
Environment is a factor. Personality is a factor. Susanne was as stubborn as a stone wall. She was also born at the wrong time. I have a twin sister and a brother 10 months older, all of us born before our parents came of drinking age. (Old fathers are likelier to produce a child who develops schizophrenia, but Susanne had a young father.) We were “the three big kids.” As children, we ignored Susie, excluded her, looked down on her. We denied her entrance to our forts, museums, and hideouts in the woods. And we lived way out in the country. We were her only playmates. Did we drive her crazy?
“I was a battered child,” she once said to me. And then I remembered. We rural children would walk home from where the school bus let us off, at the end of our mile-long dirt lane. The whole way home, our brother would verbally torment Susie. Upon arriving at the house, out in the yard, he would curl his fist and beat her repeatedly in the stomach. (No blame. He was a child, too, and our stressed-out parents with their four children were in their early 20s.) If I recall correctly these events of 60 years ago, my sister and I would stand by doing nothing, feeling nothing. We did not participate, we did not enjoy, but we felt blank. Passive. It did not cross our minds to report to our parents. I don’t think we put it through any thought process whatever. One study found that children severely traumatized in childhood are three times as likely to become psychotic in adulthood. So, stressful, traumatic childhood—check. Later, I became Susie’s passionate defender. By the time we were in our 20s, we were close friends. I spent years trying to make up for her terrible childhood. We all did. But who could possibly make up for that?
In high school, though, Susanne got good grades and had good friends and she was happy. In the Peace Corps in Liberia she was happy. She and her best friend, Sheila, lived in a rural community and taught children. The two friends gabbed incessantly and laughed a lot. Susanne took high-quality black-and-white photographs of the place and its people. That year she married the love of her life. She and her husband moved to Providence, Rhode Island, where she taught kindergarten and made crafts and baked bread and made yogurt and played the recorder. She had a good life.
Paranoid schizophrenia coincided with the stress of divorce. Still, throughout her mental illness, Susanne loved art therapy and created serene-looking still lifes, watercolors. She hooked up for a time with a postdivorce boyfriend, a sweet man.
It was Susanne’s fate to die in the woods. But recovery is being more and more talked about, and a certain number of people with the disease do recover, about 10 to 20 percent, according to even the most skeptical estimates. A model 1987 longitudinal study of 269 patients suffering from severe schizophrenia and released from the Vermont State Hospital between 1955 and 1960 found that one-half to two-thirds of them had significantly improved or fully recovered. These were the most hopeless back-ward cases. These patients had benefited from social workers and therapists and employment counselors—an extensive support system continuing over several years and consisting of one essentially unchanging professional team. By the time of the study, a significant number of them had reintegrated into the community.
Now, though, following our national deinstitutionalization policy, carried out without the community support that was supposed to go with it, our mental health care system has disintegrated. According to the devastating picture drawn by Torrey in American Psychosis, at least 20 percent of prison inmates and about a third of homeless people are severely mentally ill. Our system of non-care is, by the way, ultra-expensive.
Recovery from schizophrenia is possible. Living a meaningful life with a diagnosis of schizophrenia is possible. This is the message I wish to leave. I only wish Susanne could have heard it.