The Well Curve
Tropical diseases are undermining intellectual development in countries with poor health care—and they’re coming here next

“Mind, independent of experience, is inconceivable.”
—Franz Boas
On a bright June day in 1963, I cowered, popcorn forgotten, as The Birds unleashed a terrifying spectacle of nature gone mad. Gulls ceased to swoop and pirouette and instead careened mindlessly, joining crows in dive-bombing terrified pedestrians, children, and famously, Tippi Hedren. Their songs, their precise balletic fishing skills, and their intricate long-distance flight patterns seemed forgotten, along with their fear of people, and no one knew why. I had goose bumps, and not from the overzealous air-conditioning.
It was the sudden unexplained loss of avian intelligence that chilled me most. Hitchcock violated the era’s science fiction conventions by declining to supply the usual pat explanation from a pipe-smoking celluloid scientist, and he even omitted the conventional “The End” credit, which would have consigned the film’s grim scenes to the realm of fiction. Instead, a disquieting sense of realism prevailed—the implicit threat that the mindless fury could happen again.
I’m glad I didn’t know then what I know now. Hitchcock’s nightmare scenario is not imaginary but real, based on events that directly threaten humans as well. Hitchcock, who was fond of bird watching, two years earlier had visited California, where on August 18, 1961, thousands of Puffinus griseus seabirds, called sooty shearwaters, alighted from the northeast to fish and feast on krill. Each year they followed the California Current from the southwestern Pacific, but that year they had suddenly abandoned their fishing and coordinated flight patterns to begin suicidal dives into the rocks, dirt, and beachcombers on the north end of Monterey Bay. In the town of Capitola, birds hurled themselves into buildings and people, and died on the wing while projectile-vomiting the anchovies on which they had also feasted.
It’s unclear whether Hitchcock witnessed this mayhem himself, but accounts agree that he read of it in the newspaper. Learning this, I understood Hitchcock’s decision to depart so dramatically from the English writer Daphne du Maurier’s war allegory “The Birds,” from which the film was ostensibly adapted but to which it bore little resemblance—a choice that infuriated her. The film more closely resembles the Monterey events of 1961.
Various unsatisfying explanations for the avian degradation were proffered, including overfishing, oil spills, and confusion caused by heavy fog. But this was far from being an isolated event: for millennia, animals have suddenly lost their gifts for navigation and social organization. In the 1990s, along the same stretch of California shore, pelicans and about 400 sea lions succumbed to a mysterious stultification, abandoning their orderly behavior and losing the ability to feed and swim. They too had become stupid en masse.
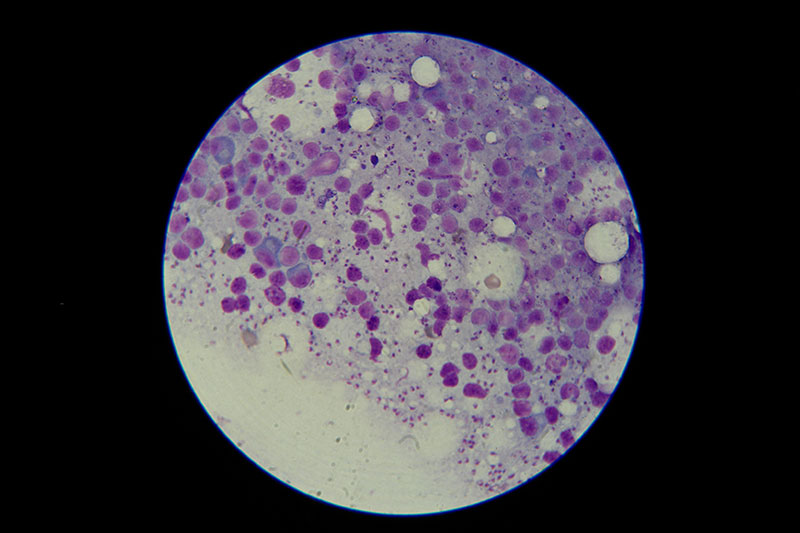
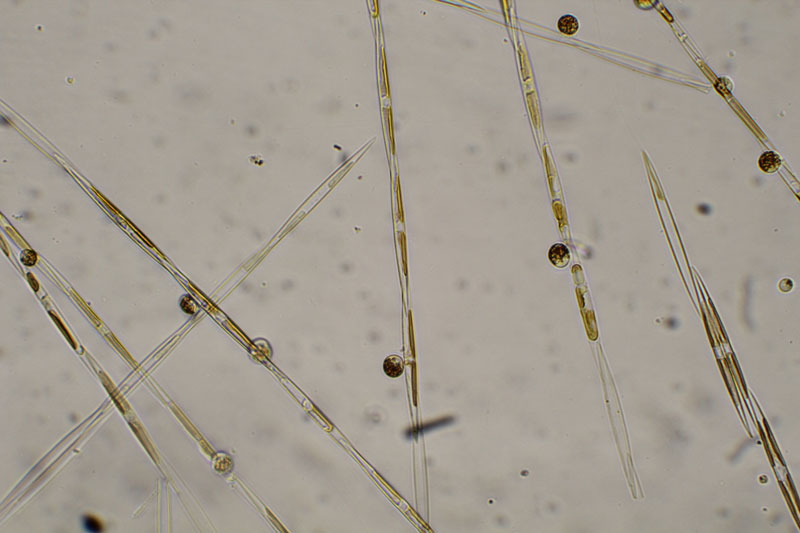
People are not immune to these strange reactions. In 1987, more than 100 Canadians developed similar symptoms after dining on tainted mussels harvested off Prince Edward Island. Short-term memory loss accompanied vomiting and diarrhea. The victims also became disoriented and aggressive and finally were wracked by prolonged crying jags. This new disease, christened “amnesiac shellfish poisoning,” was caused by the same microbe that triggered the Monterey Bay outbreaks—several species of Pseudo-nitzschia algae. The algae produce domoic acid, a powerful neurotoxin that destroys the ability to make memories and thrives in algal blooms—popularly called red tides—that are incubated by warm weather.
Tests on the remains of the Monterey Bay seabirds, anchovies, sea lions, and brown pelicans found high levels of domoic acid, which kills neurons in the hippocampus, a seat of memory. Domoic acid resembles a form of the neurotransmitter glutamate so closely that sufferers’ brains could not discern the difference as it passed through the blood-brain barrier to cause confusion, disorientation, seizure, coma, and sometimes death. Monterey Bay National Marine Sanctuary scientists announced a red tide recurrence as recently as June, followed by a mass die-off of infected anchovies, which also threatened their mammalian predators, including man.
The Microbial Mind
Pseudo-nitzschia is just one of many pathogens that erode human intelligence. As I prepared my new book, Infectious Madness, I interviewed scientists working on the effects of infections on mental health. Susan Swedo, chief of the pediatrics and developmental neuroscience branch at the National Institute of Mental Health, researches the role of Group A strep infections in children in rapid-onset cases of obsessive compulsive disorder, anorexia, and Tourette syndrome. Other visionary researchers, such as E. Fuller Torrey, executive director of Maryland’s Stanley Medical Research Institute, and Robert Yolken, director of developmental neurovirology at Johns Hopkins University, have for decades investigated the role of microbes in mental illness and have traced the path of viruses such as influenza and herpes simplex, among other microbes, in schizophrenia and bipolar disorder.
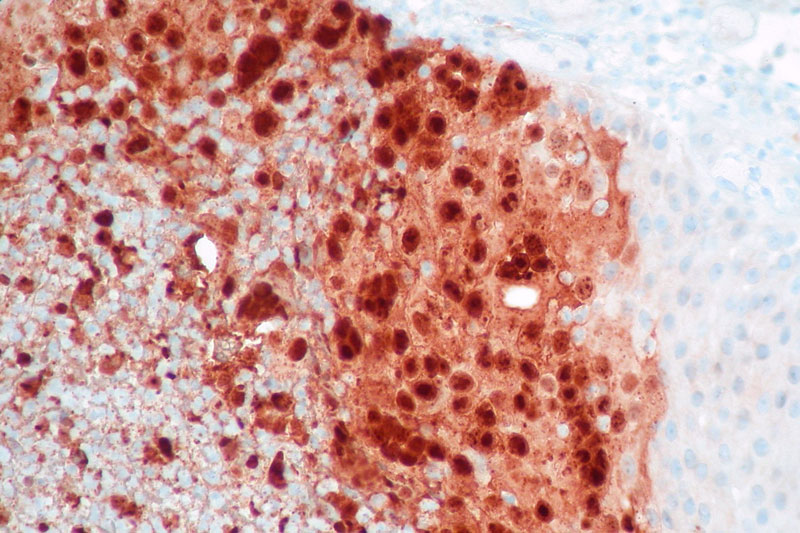
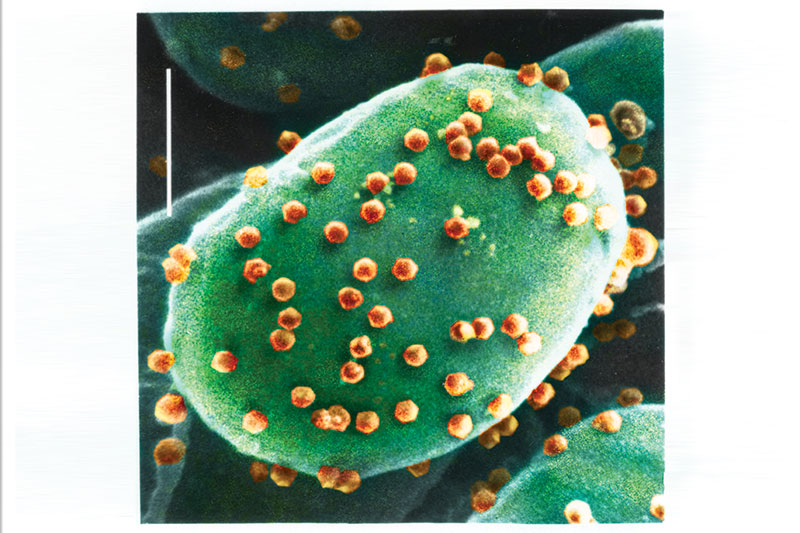
But last year, Yolken found a microbe that seems to sap intelligence, not sanity. In the October issue of Proceedings of the National Academy of Sciences, he described a study that included mental tests followed by physical screenings. Investigators from Johns Hopkins, Baltimore’s Sheppard Pratt Health System, and the University of Nebraska–Lincoln were startled to find a previously unsuspected virus, Acanthocystis turfacea chlorella virus 1, or ATCV-1, lurking in the throats of two of every five of their Baltimore research subjects.
Despite the decades Yolken has spent analyzing microbes and mental health, this finding astonished him. “It’s something that we wouldn’t have suspected would actually have any effect on humans or animals,” he told me. For one thing, ATCV-1 is a chlorovirus, which infects algae, and viruses that transcend species usually do so in modest increments within their kingdom. Yet this pathogen scaled the evolutionary ladder in a single bound as it jumped from algae to humans.
[adblock-right-01]
But the study’s baseline cognitive tests unveiled the true shocker. When compared with those who did not harbor the virus, those infected were about 10 percent slower to make calculations and had a reduced attention span, suggesting that the virus compromised their ability to calculate, to focus, and to process visual information—disadvantages in the classroom, on the job, and in other familiar learning situations. “American Researchers Discover ‘Stupidity Virus,’ ”Newsweek trumpeted when the news got out; a more measured Wired UK headline read, “Human cognition-affecting virus discovered.”
The lowered mental functioning was independent of potentially confounding factors, including age, socioeconomic status, education, place of birth, or smoking status. Gender and race made no difference. Repeating this experiment in a larger population yielded the same results, and when the research team tested mice before and after exposing them to the virus, they found 1,000 gene changes in brain regions known to be important to memory and learning. These infected mice also took 10 percent longer to navigate a maze and showed reduced attention spans, compared with the uninfected controls. Although critics suggested that they had found not an IQ-lowering microbe but rather sample contamination, Yolken refuted this suggestion in an article in the February Proceedings of the National Academy of Sciences.
Infection and Intelligence
Pseudo-nitzschia and ATCV-1 join a panoply of microorganisms that have long been suspected, and sometimes known, to change how well we think. These newcomers are getting attention because they struck in the West, where a functional public health infrastructure allows for disease surveillance and the investigation of mysterious sources of disability. But pathogens that affect cognition have traditionally infected poor people of color in the developing world, so their ravages and long-term effects have been more likely to go unanalyzed and untreated. In developing countries, points out Peter Hotez, dean of the National School of Tropical Medicine at Baylor College of Medicine in Houston, infection by such pathogens is the norm, not a headline-worthy exception.
The mental effects of pathogens, including worms and other organisms that cause schistosomiasis (or snail fever), leishmaniasis (caused by sand flies), and dengue fever, have cast a long shadow over the heavily political and seemingly endless debates over race and intelligence. Studies like a 2010 report from Randy Thornhill, an evolutionary biologist at the University of New Mexico, and a 2011 research study from Carleton University in Ottawa, have strongly correlated low average IQs from various nations with high rates of infectious disease. A 2011 article Thornhill published in the journal Intelligence calculated that, in the United States, allowing for education and wealth, “Infectious disease was the best predictor of average IQ.”
Thornhill’s “parasite-stress” theory maintains that parasites sap the brain’s energy in several ways. The newborn human brain uses fully 87 percent of the body’s “metabolic budget,” an amount that diminishes with age and maturity, and if a young brain cannot meet these initial high-energy requirements, its growth and development suffer. Microbes and larger parasites drain this energy by feeding on tissues and lodging in the digestive tract, where they siphon off nutrients and iron. Additionally, viruses divert energy from their hosts to crank out copies of themselves. This stolen energy normally would fuel brain building and other metabolic needs of the child.
The result, said Thornhill’s 2011 article, is that across the United States, “there is a negative association between infectious-disease stress and average intelligence” as measured by IQ score. To calculate the effects of disease on intelligence outside the United States, Thornhill used data from Richard Lynn and Tatu Vanhanen’s 2006 book IQ and Global Inequality, which listed average IQ scores for more than 113 countries. These ranged from a high average of 107 in Hong Kong to a low of 63 in Ethiopia. The lowest IQs were found in the poorest countries of Africa, and the authors suggest that the differences were heritable but partly due to variations in the wealth of nations.
Scientists who, like Lynn, believe in heritable racial difference in cognitive ability talk of intelligence, but they measure IQ. Moreover, they tend to conflate the two, even though many cultural and socioeconomic factors separate them. No consensus on the definition of intelligence exists: valuable intelligence varies with culture. IQ tests assess only some components of mental ability and achievement, those that are highly valued and frequently practiced in affluent Western culture, and they do so inconsistently.
Brink Lindsey, the author of Human Capitalism: How Economic Growth Has Made Us Smarter—and More Unequal (2013), cogently argues in a May 2013 web article from The Atlantic, that whatever aspects of intelligence IQ tests measure, these factors are not universal. They are assessed more accurately for affluent Westerners than for others. However, Thornhill’s analysis revealed that IQ is more closely correlated to the health of nations than their wealth.
A Panoply of Disease
One dramatic health difference between rich and poor countries is the prevalence of neglected tropical diseases, or NTDs, which afflict a billion people worldwide, most of whom live in the kind of extreme poverty that characterizes the Global South.
Apocalyptic images of dramatic medical crises such as AIDS and Ebola captivate the West and spur altruism, but when it comes to the NTDs that chronically compromise health and challenge mental abilities, our myopia has been profound. Ebola-racked Guinea, Liberia, and Sierra Leone also harbor the highest-known concentrations of hookworm victims. Since 2013, 11,000 people have died from Ebola in sub-Saharan Africa, but 10 million people—nearly half the population of these countries—suffer from at least one NTD or malaria or both. And NTDs plague extremely poor denizens of the subtropics not only of sub-Saharan Africa, but also of Saudi Arabia, Brazil, India, China, Indonesia, and Mexico. They are, in the words of Peter Hotez, the dean at Baylor, “great disablers rather than killers.”
Yet the HIV disease prevalent on the African continent and throughout the developing world deranges thinking, too. Children who acquire HIV prenatally from their mothers risk central nervous system disease that can cause a spectrum of brain dysfunction from encephalopathy to subtle cognitive impairment. Language disorders and developmental delays can result because HIV crosses the blood-brain barrier to contribute to various types of neuronal injury. A 2010 longitudinal study published in the journal AIDS examined more than 300 HIV-positive children with an average age of 12 and found that they fell into the low-average scale for memory, speed of processing, and verbal comprehension. The researchers suggested that neurodevelopmental problems in children and adolescents with HIV might be linked to “changes in proinflammatory monocytes”—immune-system changes that the virus provokes.
Cognitive delays plague many people who are infested with parasitic worms, including 807 million–1.2 billion people with ascariasis, 604–795 million suffering from trichuriasis, and 576–740 million with hookworm infection, concentrated in sub-Saharan Africa, Asia, and Latin America. Each of these diseases hinders economic prosperity by decimating the workforce.
[adblock-left-01]
What’s more, treatment does not necessarily restore the infected person to mental vigor. In a 1997 study of 196 Jamaican schoolchildren infected with whipworm, children who had been treated with antiparasitic medication were compared with those who had received a placebo and with others who remained untreated. The infected suffered impaired performance on reasoning and memory tests, but not in attention or fine motor skills. Even the children who had been treated showed these deficits, suggesting that removing the parasite is not enough. Treatment must also include focused efforts to restore lost cognitive functioning.
Young sub-Saharan residents are alarmingly vulnerable to drastic reduction in IQ (employed, as usual, as a marker for intelligence) due to malaria and other infections. This is because, Thornhill and his colleagues theorize, “From an energetic standpoint, a developing human will have difficulty building a brain and fighting off infectious diseases at the same time, as both are very metabolically costly tasks.”
Only malaria infects more people than schistosomiasis, also known as bilharzia or “snail fever.” Freshwater snails carry this parasitic disease, which afflicts at least 261 million people, mostly in sub-Saharan Africa but also in 77 other countries, including Brazil. Onchocerciasis, also known as river blindness, infects 30 million people in sub-Saharan Africa, causing skin nodules, debilitating itching, and blindness. The parasite is transmitted by the river-dwelling Simulium blackfly. Leishmaniasis and Chagas disease infect 10 million and 7.5 million people, respectively, in Mesoamerica. “Many of these diseases are stigmatizing and they produce mental anguish in this manner, too,” adds Hotez. Parasites carried by both dogs and cats can cause cognitive and intellectual deficits, as well as epilepsy, blindness, and impaired lung function, and are also implicated in schizophrenia.
Diarrhea is a common symptom of microbial and parasitic infection. Thornhill noted in a 2011 Institute of Medicine report that “if exposed to diarrhoeal diseases during their first five years, individuals may experience lifelong detrimental effects to their brain development, and thus intelligence. Parasites may [also] negatively affect cognitive function in other ways, such as infecting the brain directly.”
Tuberculosis was once the leading cause of death in the United States. Today, Nigeria has the fourth-highest tuberculosis rate in the world, with more than 400,000 cases per year. Moreover, it manifests as a different disease in the developing world than in the West. Although we commonly associate tuberculosis with the lungs, it can attack many sites in the body. When it invades the brain, causing tuberculosis meningitis, sufferers are left with severe brain damage. This outcome accounts for just one percent of cases in the West, but 14 times as many in Nigeria. TB-HIV synergy leaves one in every five of the country’s TB survivors severely brain damaged.
It’s Happening Here
Beginning in 2008, lurid headlines screamed about “The Worms That Invade Your Brain,” “Worm Removed From Woman’s Brain,” and “Hidden Epidemic: Tapeworms Living Inside People’s Brains.” Cysticercosis had hit the United States with a vengeance. MRIs of patients in emergency rooms with sudden epilepsy or fainting revealed that their brains were irregularly studded with tapeworms. That’s right, tapeworms. Although we think of them, when we must, as infesting the human digestive system, where well-nourished specimens can grow to 20 feet or more, these people suffered instead from a condition known as taeniasis. Each worm produces about 50,000 eggs, which are shed in the feces of infected people. Once on the ground and eaten by pigs, they grow into larvae that normally burrow into the porcine blood vessels, where they wait to be consumed by humans eating undercooked pork, and their life cycle begins again.
But sometimes the eggs take a fateful detour when accidentally ingested by another human, as when an infected person prepares food without washing his hands. Then, an egg develops into a larva that burrows into the human bloodstream and hitches a ride to the brain. Tunneling into the brain, the larvae become encysted, cloaking themselves from the immune system with specialized tissues. Thus ensconced and unmolested by the immune system, they unleash the horribly versatile disease called cysticercosis.
Cases are more common than one might think. Ted Nash, chief of the gastrointestinal parasites section at the National Institutes of Health, told Discover magazine in 2012, “Minimally, there are 5 million cases of epilepsy [worldwide] from neurocysticercosis.” From 1,500 to 2,000 neurocysticercosis cases have been diagnosed in the United States when confused, unconscious, or epileptic patients are brought to the hospital and the detection of antibodies definitively identifies the disease. Cysts near the brain’s visual cortex can blind the carrier. Cysts near the language area can disrupt speech or comprehension. Cysts sometimes block the flow of cerebral fluid, causing hydrocephalus, which necessitates a shunt to relieve the pressure and prevent unconsciousness and death. All too frequently, a tapeworm cyst causes epilepsy.
Treatment may not save the intellect because although the drug praziquantel kills the larvae, it also unleashes a vigorous immune response, “friendly fire” that ends up harming the brain. Most studies show that with many if not most such worm-borne pathogens, deworming arrests the cognitive decline but does not restore lost intellectual functioning.
Such disastrous cases are only the most dramatic manifestation of an epidemiological sea change: tropical diseases—and their neglect—are not limited to the tropics any more. They’re now very much at home in the United States. The Big Five diseases—Chagas disease, cysticercosis, toxocariasis, toxoplasmosis, and trichomoniasis—are quite common here among the poor, Hotez says. “While sub-Saharan Africa accounts for many of the world’s NTDs, somewhat paradoxically, most of the world’s NTDs can be found among the poor living in wealthier countries, including the ‘Group of 20’ nations. Houston and Texas … represent ‘ground zero’ for many of America’s neglected tropical diseases.”
In addition to life-threatening heart and respiratory devastation, this suite of communicable neuropsychiatric conditions saps the brainpower as well as the strength of poor people of color at home, just as it does abroad. Yet many doctors in the United States remain in denial. When the patient of a doctor at the Baylor College of Medicine received a letter saying that blood he had donated was being rejected because of a positive test for Chagas disease, the doctor exploded, “The test is wrong. That disease doesn’t exist in the United States!”
But it does, and this troubling scene is replayed across the country as American blood donors learn that they have a Third World disease. Tropical medicine experts agree that at least 330,000 U.S. citizens have Chagas disease, the most common parasitic disease in the Americas, and estimates range as high as one million. It infects six million to seven million more people in Latin America. This chronic, silent parasitic infection leads to fatal heart or intestinal damage in two of every five sufferers, and it also causes intellectual slowing. It can be treated, but the lack of awareness by doctors in the United States means that it often isn’t.
The insect vector for Chagas is an unwelcome immigrant—the triatomine or “kissing” bug, which lives in the cracks of substandard housing and passes on the parasite to people by defecating while sucking their blood. Chagas causes as many as one in 10 neurological problems in Mesoamerica. In the United States, it mainly affects poor Hispanic communities, but taken altogether, the infections that ravage the developing world now imperil the bodies and minds of at least 14 million U.S. residents.
Blame the Climate
Why are tropical diseases flourishing here? Xenophobes may indict immigrants who bring microbes north with them, but the real culprit is the U.S. climate. Many microbes function only within a narrow temperature range, and the life cycles of the parasites in question often require heat. This country obliges with temperatures that are considerably warmer than those in much of the affluent West, particularly those in northern Europe. “The U.S. is somewhat unusual in being a wealthy nation much of whose population lives in very warm, humid regions,” Stan Cox, a senior scientist at the Land Institute, told The Washington Post in July.
Climate change promises to accelerate the spread of tropical and subtropical diseases, because warming encourages the growth of parasite vectors such as mosquitoes, which will put another two billion people at risk of the mosquito-borne dengue fever virus by 2080. DDT spraying had all but banished dengue in the United States in the 1950s, but the pesticide was banned in the 1960s, and in 2003, dengue made a comeback in Houston. Higher temperatures encourage the snails that carry schistosomiasis and the sand flies that carry leishmaniasis to expand their territory. Meteorological events have also brought NTDs home. The insects that carry Chagas disease proliferated in Louisiana after Hurricane Katrina in 2005, and clouds of African dust borne on winds at an altitude of 15,000 feet constantly traverse the Atlantic to scatter bits of the Sahara Desert, and its microbes, over front yards and playgrounds in the Americas. In 2001, U.S. Geological Survey scientists determined that “hazardous bacteria and fungi hitchhike across the Atlantic on North African dust plumes.” Expect higher disease rates in the wake of these plumes.
The High Cost of Infection
Twenty million Americans are not just poor, but profoundly so: 1.65 million households live on less than $2 a day. The 20 million includes 3.55 million children who suffer lifelong disability from malnutrition and infections that reduce vigor and lifetime productivity and thus help perpetuate poverty.
What’s more, the poorest states are all in the warmest part of the country. This includes urban sites, where many infections thrive and gain virulence in the sort of overcrowded conditions commonly found in cities. The nation’s poorest major metropolitan area, McAllen-Edinburg-Mission, Texas, and the nation’s poorest smaller cities, all in the South, are marred by inadequate sanitation, environmental contaminants, and overcrowded substandard housing. They are also often home to ethnic enclaves of African Americans and other minorities. As Hotez points out, when dengue fever struck Houston, the poorest parts of the city were the most profoundly affected areas, but not one patient was accurately diagnosed, including the two people who died.
Our warm climate, poverty, and inequitable access to medical care make NTDs a problem largely confined to the United States among wealthy nations, one that targets pockets of poor African Americans, Hispanics, and immigrants. We’ve long known, for example, that HIV is largely a disease of poor people of color in the United States, just as it is in Africa. What’s less well known is the cognitive cost of HIV and other infections.
A July report in Pediatrics by University of Michigan scholar Nicole Hair analyzed MRI scans from poor young people ages four to 22 and determined that those living in poverty had test scores lower than their wealthier peers and developmental lags in their brain development. The MRIs found the volume of their brains’ gray matter measured eight to 10 percent below the developmental norm for their age.
“We used to think of poverty as a social policy issue in the U.S., but now it appears to be a biomedical issue,” says Seth Pollak, a developmental psychologist at the University of Wisconsin–Madison. Although NTDs tend to strike people of color, “These are diseases of poverty,” insists Hotez. “Why poverty promotes neglected parasitic infections is unknown, although factors such as poor housing and sanitation and environmental contamination are likely contributors, while so far the links to ethnicity appear to be mainly socioeconomic.”
This take on race, intelligence, illness, and poverty is the exact opposite of hereditarian screeds, from Arthur Jensen’s “Thirty Years of Research on Black-White Differences in Cognitive Ability” to Charles Murray and Richard J. Herrnstein’s The Bell Curve to J. Philippe Rushton’s musings on race, intelligence, and penis size. These broadsides and their refutation have dominated the public debate on race and intelligence. The authors’ theories rest on several articles of faith. One is that intelligence, measured by IQ tests, is largely genetic and varies in a racial hierarchy, with Asians or Caucasians usually occupying the apex and various African groups located at the bottom. They also believe that these racial differences are maintained because IQ is genetic and immutable, so racial gaps are persistent and an adult retains the same IQ throughout his life.
Satoshi Kanazawa of the London School of Economics has addressed the role of pathogens in intelligence via claims of reverse causality. Writing in the British Journal of Health Psychology, Kanazawa argued that the excess illness of people in the developing world is caused by lower intelligence, rather than the other way around. Among the flaws in his argument are dubious IQ scores and the assertion that IQ scores are immutable.
But James R. Flynn’s 2012 book, Are We Getting Smarter? Rising IQ in the Twenty-First Century, demonstrates that IQ measures not innate intelligence but rather specific acquired skills. Most notably, he found that IQ scores have risen about three points a decade in the United States and countries like it. The Flynn effect can’t be explained genetically, and the claim that genetics prevents low African IQs from rising is belied by a 14-point increase in Kenyan IQ tests between 1984 and 1998, a gain largely ascribed to improvements in health.
The illogical belief of hereditarians that intelligence is immutable invokes futility, which supports recommendations that we devote no resources to ameliorate the intelligence gap between the developed and the developing world, because nothing can be done. But our expanding understanding of the effects of disease on intelligence offers hope, and some evidence, such as the Flynn effect in Kenya, that the problem is solvable—that quelling disease can raise intelligence levels.
A powerful argument exists, then, for ending the erosion of intelligence by pathogen exposure, but how can we best do it? “Being smart is the most expensive thing we do,” biologist Christopher Eppig, then of the University of New Mexico, wrote in 2011, adding, “Not in terms of money, but in a currency that is vital to all living things: energy.” Shoring up intelligence is likely to be expensive in terms of money as well, however, because, Eppig told a journalist in 2012, “a social policy aimed at elevating IQ would want to focus on reducing the infection rates and durations of the infections that are most costly to the brain, which we predict include malaria, diarrheal diseases, tuberculosis, and intestinal worms.”
Treatment Strategies
Medications would play an important role, but the pipeline is drying up. A 2011 European College of Neuropsychopharmacology report warns that “research in new treatments for brain disorders [are] under threat” as corporate behemoths including Roche, Pfizer, AstraZeneca, and GlaxoSmithKline eliminate teams, cut funding, and shutter divisions dedicated to psychiatric drugs. Big Pharma has also largely abandoned the development of antibiotics, which have decreased in number over the past 20 years, though there seems to have been a small recent uptick. Pfizer, which once developed more antibiotics than anyone, closed its antibiotic research division in 2011. In February, The New York Times speculated that few of the 40 antibiotics currently in development were likely to emerge as FDA-approved drugs.
These are unfortunate developments, but prevention is often better than medication. “The most important thing, if you want to deal with mental disorders, is to prevent them from happening in the first place,” Alan S. Brown, a professor of psychiatry and epidemiology at Columbia University Medical Center, told Scientific American Mind in 2008.
The dwindling stores of medications are not the only reason why prevention is superior to drugs. Mental symptoms and diseases are among the side effects of many treatments. Doxycycline for malaria causes anxiety, depression, and hallucinations. Interferon for hepatitis C can cause or worsen depression, and HAART, drug regimens against AIDS, can cause paranoia, hallucinations, and catatonia, turning patients into mute, immobile “living statues.” And as we’ve seen, even safe, effective treatments yield limited results because infection-associated brain damage cannot always be reversed.
This makes the development of vaccines for the developing world and poor enclaves of the United States critically important. The Sabin Vaccine Institute, for example, is already testing new vaccines against schistosomiasis and hookworm in clinical trials in Brazil and Gabon. Closer to home, Hotez is developing vaccines with funding from the United States and Japanese governments and from institutions such as the Gates Foundation, which have already funded some needed vaccines.
But we need to know even more, says Robert Yolken of Johns Hopkins, reminding us that immense numbers of the mentally ill in poor and developing nations go undiagnosed. Moreover, we are not even aware of many pathogens that undoubtedly exist in such areas and may also cause cognitive problems.
From the mutual contagion of immigrants and citizens, to the changes in our climate, which grows ever more welcoming to subtropical pathogens, to the African winds blowing microbes our way, to the already sickened ethnic enclaves within our borders, the problem must be addressed on purely communitarian grounds. Treatment and prevention are not optional. Selectively withholding care from poor people of color is indefensible on ethical grounds, but self-interest also demands that we address NTDs, because these are now U.S. diseases. Our medical interdependence makes this everyone’s problem.